 Congratulations to our amazing Lactation Consultants!!!
Congratulations to our amazing Lactation Consultants!!!
Breastfeeding – Lactation Consulting
 Our pediatricians at Forest Lane Pediatrics of Dallas, Frisco and Mesquite work closely with our Board Certified Lactation Consultants to support breastfeeding mothers in order to help all newborns, infants, and children. Even if you have decided not to breastfeed, or you are medically unable to do so, our lactation consultants want to help you with questions regarding preparation of formula, baby care and most importantly, support for your family! We strive to provide outstanding pediatric care for the families throughout the Dallas/Fort Worth metroplex who entrust their child’s well-being to our experienced team of board-certified pediatricians and lactation consultants. Below, please find some frequently asked questions & answers from our new Moms and Dads.
Our pediatricians at Forest Lane Pediatrics of Dallas, Frisco and Mesquite work closely with our Board Certified Lactation Consultants to support breastfeeding mothers in order to help all newborns, infants, and children. Even if you have decided not to breastfeed, or you are medically unable to do so, our lactation consultants want to help you with questions regarding preparation of formula, baby care and most importantly, support for your family! We strive to provide outstanding pediatric care for the families throughout the Dallas/Fort Worth metroplex who entrust their child’s well-being to our experienced team of board-certified pediatricians and lactation consultants. Below, please find some frequently asked questions & answers from our new Moms and Dads.
Lactation Consultant
Janis Wilbert, BA, CLC, IBCLC
Breastfeeding and Pumping: 7 Tips For Success
Breastfeeding FAQs
Newborn/Infant Frequently Asked Questions
How often should I breastfeed?
Early and often! Breastfeed as soon as possible after birth, then breastfeed at least 8 to 12 times every 24 hours to make plenty of milk for your baby. This means that in the first few days after birth, your baby will likely need to breastfeed about every hour or two in the daytime and a couple of times at night. Healthy babies develop their own feeding schedules. Follow your baby’s cues for when her she is ready to eat.
How long should feedings be?
Feedings may take 10 to 20 minutes or longer per breast, but there is no set time. Your baby will let you know when he or she is finished. If you are worried that your baby is not eating enough, talk to your baby’s doctor.
What are signs of a good latch?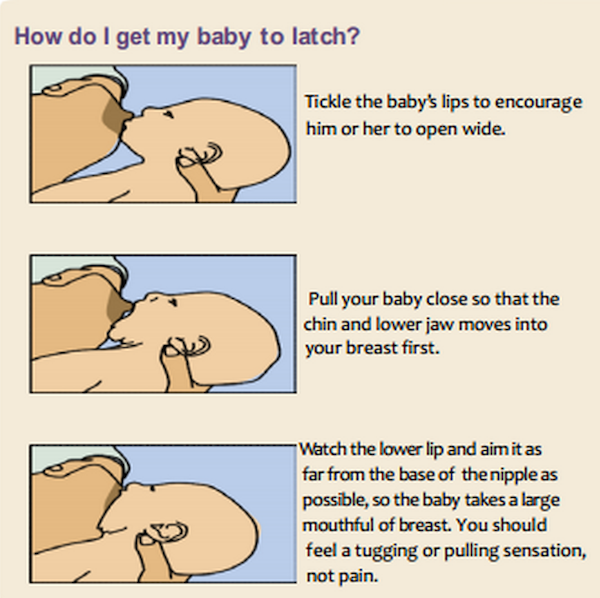
- The latch feels comfortable to you, without hurting or pinching. How it feels is more important than how it looks.
- Your baby’s chest is against your body and he or she does not have to turn his or her head while drinking.
- You see little or no areola, depending on the size of your areola and the size of your baby’s mouth. If areola is showing, you will see more above your baby’s lip and less below.
- When your baby is positioned well, his or her mouth will be filled with breast.
- The tongue is cupped under the breast, although you might not see it.
- You hear or see your baby swallow. Some babies swallow so quietly, a pause in their breathing may be the only sign of swallowing.
- You see the baby’s ears “wiggle” slightly.
- Your baby’s lips turn out like fish lips, not in. You may not even be able to see the bottom lip.
- Your baby’s chin touches your breast.
How do I position my baby during feeding?
Hold your baby close, next to your skin, tummy to tummy. Press his chin into your breast with your nipple just opposite his nose. Tickle the baby’s upper lip with your nipple to make his mouth open wide, like a yawn. Hold your hand behind the baby’s neck and shoulders. This will allow the baby to tip his head back so he can open his mouth wider. Use your other hand to support the breast and compress it slightly in the same direction as his lips. This will help him to get more of a mouthful. When your baby’s mouth is wide open, bring him to your breast quickly to help baby get more breast into his mouth. Baby should latch onto the areola, not just the nipple. This will enable baby to get more milk. If you feel discomfort with nursing, the baby may not have enough breast tissue in his mouth. Insert your finger between his jaws and the breast tissue to break suction, and then re-latch.

Breastfeeding positions:
- Cross-cradle: Hold baby tummy to tummy. Hold your forearm along baby’s back, with your hand supporting baby’s neck and shoulders. Your other hand supports the breast like a U.
- Football: Baby’s body is under your arm and your hand supports his neck and shoulders. Baby’s head is under the breast, looking up at you. Your other hand supports the breast like a C.
- Side lying: You can rest while your baby feeds! Lay on your side, baby tummy to tummy with you. Use your upper arm to support your breast in a C hold.
When baby’s mouth opens wide, press baby onto breast with your lower hand between baby’s shoulder blades. Another way is to hold your body up on one elbow. Place baby on her back, under your breast and use your upper hand to support the breast in C hold. Tickle the baby’s lip to get a wide gap then lower your breast into baby’s mouth. Once the baby is latched and sucking, pull out your lower arm and lay on your side.
How do I prepare powdered formula?
Per the Center for Disease Control guidelines, powdered formula must be mixed with water hot enough to kill germs, and safely storing formula can prevent growth of Cronobacter bacteria and other germs. These are keys to keeping your baby safe and healthy.
- Clean up before preparation
- Wash your hands with soap and water.
- Clean bottles in a dishwasher with hot water and a heated drying cycle, or scrub bottles in hot, soapy water and then sterilize them.
- Clean work surfaces, such as countertops and sinks.
- Prepare safely
- Keep powdered formula lids and scoops clean (be careful about what they touch).
- Close containers of infant formula or bottled water as soon as possible.
- Use hot water (158° F/70° C and above) to make formula.
- Carefully shake, rather than stir, formula in the bottle.
- Cool formula to ensure it is not too hot before feeding your baby by running the prepared, capped bottle under cool water or placing it into an ice bath, taking care to keep the cooling water from getting into the bottle or on the nipple.
- Before feeding the baby, test the temperature by shaking a few drops on your wrist.
- Use quickly or store safely
- Use formula within 2 hours of preparation. If the baby does not finish the entire bottle of formula, discard the unused formula.
- If you do not plan to use the prepared formula right away, refrigerate it immediately and use it within 24 hours. Refrigeration slows bacterial growth and increases safety.
- When in doubt, throw it out. If you can’t remember how long you have kept formula in the refrigerator, it is safer to throw it out than to feed it to your baby.
How do I store prepared powdered formula?
Once opened, powder formula containers should be closed and stored in a cool, dry place — not in the refrigerator. Avoid extreme temperatures. Use contents within one month. Once mixed, feed immediately or refrigerate in a sealed container, and use within 24 hours. See the label for specific instructions. Do not leave prepared formula at room temperature and do not freeze it, because doing so can cause the protein and fat to separate. If your baby does not finish a bottle of formula within one hour, throw it away. Do not save it for later. During a feeding, your baby’s saliva can contaminate the formula in the bottle. Once this occurs, reheating or refrigerating will not kill the bacteria. If you warm the formula and your baby decides not to take it, do not refrigerate it and reheat it again later. Throw it out instead.
How do I store my breast milk?
How often should I make my baby’s bottles?
Some parents opt to make a bottle just before each feeding, but many others choose to pre-make and refrigerate enough to use for the day. If you know your baby eats every 3-4 hours, for instance, you can make six to eight bottles to last you all day. Mix your baby’s formula in 2 or 3-ounce (60- or 90-milliliter) servings for the first few weeks and gradually increase the amount as you become familiar with your baby’s eating patterns and appetite. Remember to refrigerate it immediately after mixing. If your baby is staying with a caregiver for a long period of time, you may want to prepare just one or two bottles and leave instructions and supplies (bottles, nipples, formula, and water, if necessary) so the caregiver can prepare bottles as needed and not waste any formula. After all, you’ll need to throw away any mixed formula after 24 hours.
Is my baby eating enough?
Babies grow at different rates, and at times you may wonder whether your baby is getting enough nutrients to develop properly. Here’s a general look at how much your baby may be eating at different stages:
- On average, a newborn consumes about 1.5-3 ounces (45-90 milliliters) every 2-3 hours. This amount increases as your baby grows and is able to take more at each feeding.
- At about 2 months, your baby may be taking 4-5 ounces (120-150 milliliters) at each feeding and the feedings may be every 3-4 hours.
- At 4 months, your baby may be taking 4-6 ounces (120-180 milliliters), depending on the frequency of feedings and his or her size.
- By 6 months, your baby’s formula intake can be between 24-32 ounces (720-950 milliliters). This also depends on whether you’ve introduced any baby food.
What should I expect for the first 6 weeks?

What are hunger cues? How do I know when my baby is hungry?
Babies show several cues in readiness for breastfeeding. Tuning into your baby’s cues will make your feeding more successful and satisfying for both your baby and for you. Your baby does not have to cry to let you know he is hungry. Crying is the last hunger cue! Here are a few of the most common hunger cues.
- Awakening Soft sounds
- Mouthing (licking lips, sticking tongue out, licking lips)
- Rooting towards the breast (turning the head and opening the mouth)
- Hand to mouth activity
- Crying beginning softly and gradually growing in intensity
What is skin-to-skin contact? Why is it important?
Skin-to-skin contact is the close contact includes the baby unwrapped down to their diaper and tucked under mother’s clothing so that both mother and baby can begin or continue the attachment/bonding process. There are numerous reasons why keeping your baby right on your chest, skin-to-skin, is essential. Babies cry less and latch properly to the breast sooner. They are also able to maintain their skin temperature more efficiently, and they have a better tolerance for pain when receiving regular skin-to-skin contact.
How do I hand express breast milk?
- Position the thumb (above the nipple) and first two fingers (below the nipple) about 1” to 1–1/ 2” from the nipple, though not necessarily at the outer edges of the areola. Use this measurement as a guide, since breasts and areolas vary in size from one woman to another. Be sure the hand forms the letter “C” and the finger pads are at 6 and 12 o’clock in line with the nipple. Note the fingers are positioned so that the milk reservoirs lie beneath them.
- Avoid cupping the breast
- Push straight into the chest wall; Avoid spreading the fingers apart; for large breasts, first lift and then push into the chest wall
- Roll thumb and fingers forward at the same time. This rolling motion compresses and empties milk reservoirs without injuring sensitive breast tissue.
- Repeat rhythmically to completely drain reservoirs; Position, push, roll..; Position, push, roll…
- Rotate the thumb and fingers to milk other reservoirs, using both hands on each breast.
Avoid These Motions:
- Do not squeeze the breast, as this can cause bruising.
- Sliding hands over the breast may cause painful skin burns.
- Avoid pulling the nipple, which may result in tissue damage.
Does my baby need cereal or water?
No, your baby only needs breast milk or formula for the first 4-6 months of life. The American Academy of Pediatrics recommends exclusive breastfeeding for 6 months. Breast milk or formula alone will provide all the nutrition your baby needs. Giving the baby cereal may cause your baby to not want as much breast milk, gain too much weight, and have hard constipated stools. Even in hot climates, breastfed infants do not need water or juice.
Is my baby getting enough Vitamin D?
Vitamin D is needed to build strong bones. All infants and children should get at least 400 International Units (IU) of vitamin D each day. To meet this need, all breastfed infants consuming less than 32 ounces of formula per day should be given a vitamin D supplement of 400 IU each day. Sunlight is a major source of vitamin D, but it is hard to measure how much sunlight your baby gets, and too much sun can be harmful. Once your baby is weaned from breast milk, talk to your baby’s doctor about whether your baby still needs vitamin D supplements. Some children do not get enough vitamin D through diet alone.
Can I drink alcohol and nurse my baby?
Current research says that occasional use of alcohol (1-2 drinks) does not appear to be harmful to the nursing baby. If you are worried about the amount of alcohol in your breast milk, there are products available to test the amount of alcohol in your breast milk: www.upspringbaby.com
- The American Academy of Pediatrics Committee on Drugs classifies alcohol (ethanol) as a “Maternal Medication Usually Compatible with Breastfeeding.” The American Academy of Pediatrics Section on Breastfeeding notes: “Breastfeeding mothers should avoid the use of alcoholic beverages because alcohol is concentrated in breast milk and its use can inhibit milk production. An occasional celebratory single, small alcoholic drink is acceptable, but breastfeeding should be avoided for 2 hours after the drink.”
- Many experts recommend against drinking more than 1-2 drinks per week.
- Per Hale (2008), “mothers who ingest alcohol in moderate amounts can generally return to breastfeeding as soon as they feel neurologically normal.”
- There is no need to pump & dump milk after drinking alcohol, other than for mom’s comfort — pumping & dumping does not speed the elimination of alcohol from the milk.
- Alcohol has been shown to inhibit let-down and decrease milk production
- If you’re away from your baby, try to pump as often as baby usually nurses (this is to maintain milk supply, not because of the alcohol). At the very least, pump or hand-express whenever you feel uncomfortably full–this will help you to avoid plugged ducts and mastitis.
How do I contact the Lactation Counselor at Forest Lane Pediatrics?
Call Janis Wilbert, BA, CLC, IBCLC at 972.284.7770






